What Is Temporomandibular Joint Disorder?
Have you ever woken up in the morning and struggled to open your jaw? Or noticed a faint clicking sound right in front of your ear while yawning and brushed it off as “nothing serious”? That vague pain spreading to the temples, sometimes radiating toward the ear or teeth… Many people assume these complaints are caused by stress, fatigue, or the natural outcome of a long, tiring day. Most of the time, they are ignored with the thought, “It’ll pass in a day or two.” Yet these seemingly minor signals can actually be an important warning sent by the body.
Although the name may sound complicated, it refers to a structure we all know very well. The temporomandibular joint connects the lower jaw to the skull and allows us to speak, chew, swallow, and yawn. Throughout the day, it works hundreds sometimes thousands of times without us even realizing it. Whether we’re taking a bite of food, smiling, having a long conversation, or even clenching our teeth during sleep, this joint is constantly doing its job.
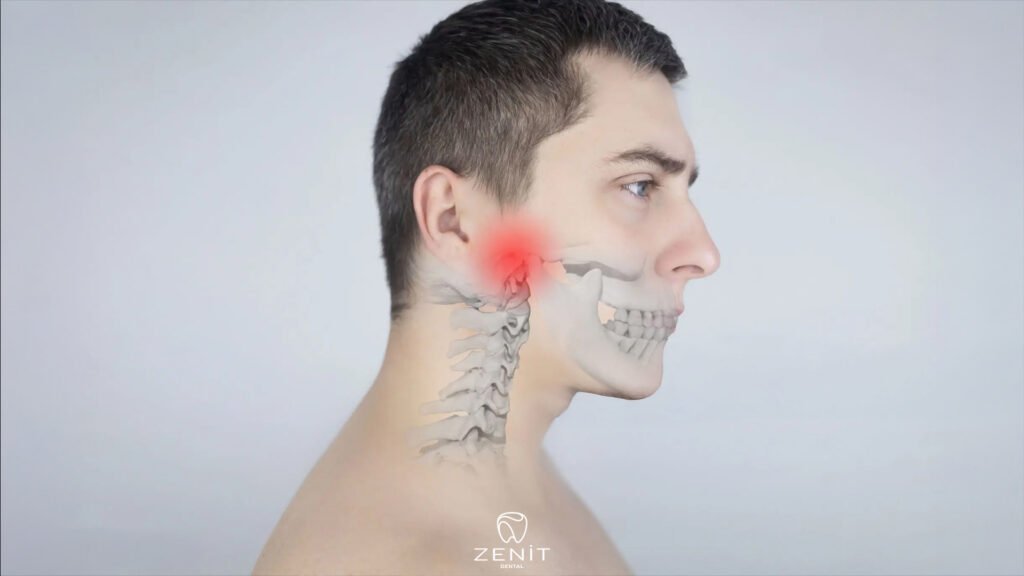
Considering how intensely it is used, it’s no surprise that this structure is quite delicate. The temporomandibular joint functions through the coordinated work of many components, including bones, muscles, ligaments, and an articular disc. When this harmony is disrupted, a chain reaction begins. Jaw pain, limited movement, clicking or popping sounds when opening or closing the mouth, headaches, neck pain, and even a sense of fullness in the ear may start to appear. What makes it more confusing is that these symptoms are not always clear or localized; sometimes they feel like tooth pain, sometimes they are mistaken for an ear problem, and sometimes they are dismissed as “just stress.”
What Is the Temporomandibular Joint (TMJ)?
Although we don’t hear its name very often, the temporomandibular joint sits right at the center of our daily lives. Located just in front of the ears, this joint exists on both the right and left sides and allows the lower jaw to move. Every time we take a bite at breakfast, talk during the day, laugh, or yawn, it is the true hero behind our jaw’s smooth movement.
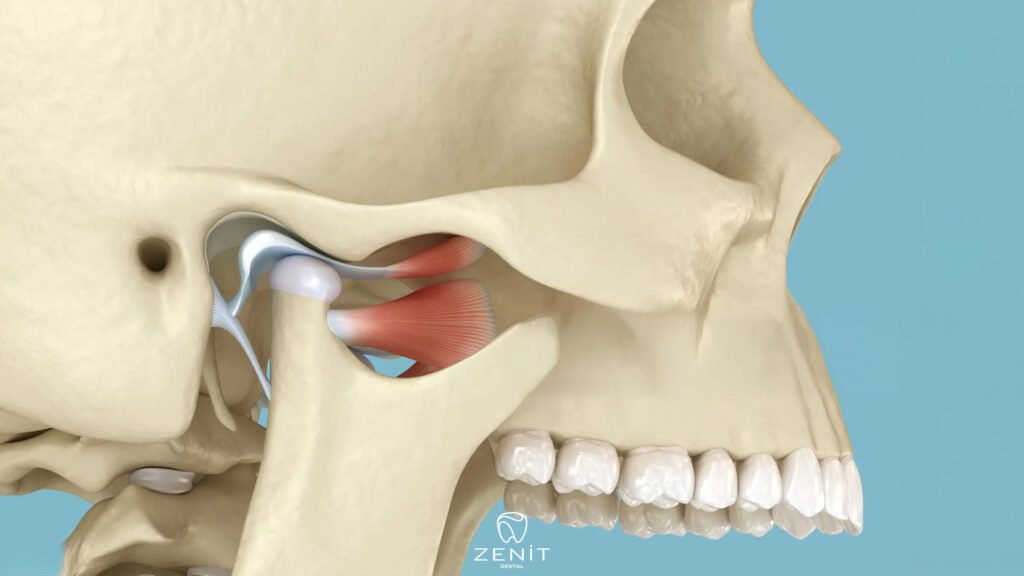
It wouldn’t be accurate to think of this joint as a simple hinge. The temporomandibular joint doesn’t just open and close; it also allows the jaw to move forward, backward, and side to side. This wide range of motion makes it one of the most complex and hardest working joints in the human body. It activates hundreds of times a day without us even noticing.
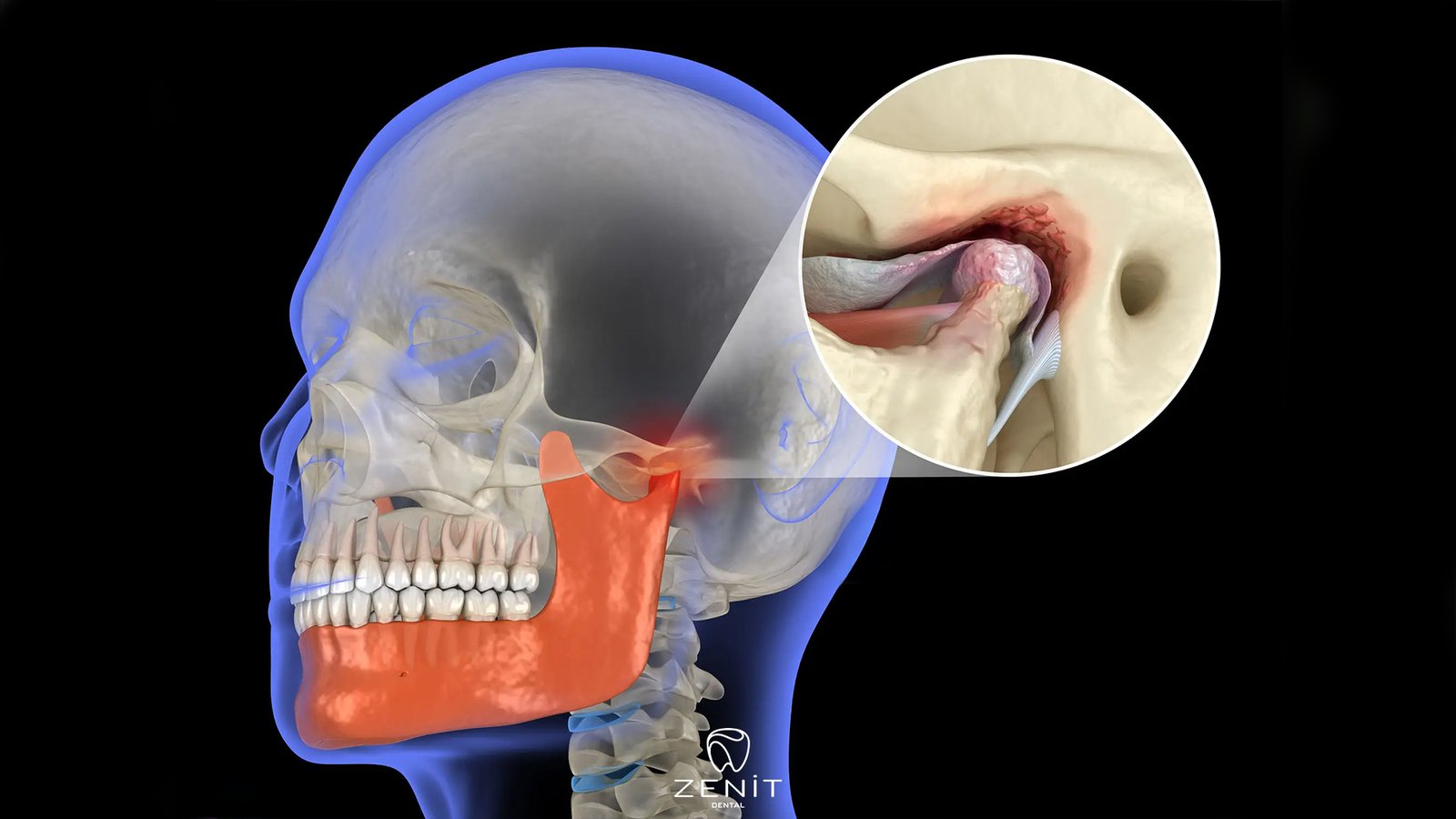
Inside the joint lies a small yet crucial structure called the articular disc. This disc acts like a cushion between the jawbone and the skull. It prevents the bones from rubbing against each other and allows movements such as chewing and speaking to be smooth and pain-free. For the joint to function properly, the disc must remain in the correct position.
The temporomandibular joint does not work alone. It functions in perfect coordination with muscles, ligaments, and nerves. As long as this balance is maintained, we experience no jaw related problems. However, factors such as stress, teeth clenching, jaw trauma, improper bite alignment, or long-term habits can disrupt this delicate harmony. And that is exactly when temporomandibular joint disorder begins to develop.
What Is Temporomandibular Joint Disorder?
Temporomandibular joint disorder is not a single condition that can be defined in isolation. Rather, it is an umbrella term covering many different problems affecting the jaw joint and the surrounding muscles. In other words, not everyone experiences the same underlying issue, but the discomfort usually makes itself known in a similar place: the jaw.
In some people, the problem is primarily muscular. Being under intense stress, unconsciously clenching the teeth, keeping the jaw tense, or maintaining poor posture for long periods can cause the muscles to become overworked and painful. In others, the issue lies within the disc inside the joint. This disc, which normally ensures smooth movement, may shift out of place or fail to move as it should. In more advanced cases, wear and tear can develop on the joint surfaces.
Regardless of the cause, the experience shares a common feeling: the jaw no longer works as comfortably as it once did. Difficulty opening the mouth, sounds during movement, quick fatigue while eating, or that familiar ache felt in the jaw by the end of the day… These are the body’s way of saying, “Something isn’t quite right.”

What Are the Most Common Symptoms of Temporomandibular Joint Disorder?
One of the most confusing aspects of temporomandibular joint disorder is that it doesn’t appear the same way in everyone. While some people feel only mild discomfort, for others it can turn into a problem that significantly affects daily life. Still, there are certain signs that many people share.
Jaw pain or tenderness is among the most common complaints. Clicking, popping, or grinding sounds heard while opening or closing the mouth are also quite frequent. Some people notice difficulty opening their mouth fully, or even feel as though their jaw occasionally locks. Ear pain, pressure, or a sensation of fullness is also common despite the absence of an actual ear problem.
In addition, headaches that spread to the temples, along with persistent tension in the face, neck, and shoulder muscles, often accompany TMJ disorder. Fatigue in the jaw while eating or pain during chewing is also widely reported. These symptoms may remain mild and go unnoticed at times, or become more pronounced during stressful periods, significantly affecting overall comfort and quality of life.
What Causes Temporomandibular Joint Disorder?
There is no single cause behind temporomandibular joint disorder. In most cases, several factors come together, and over time the jaw joint struggles to cope with the load. Unconscious teeth clenching and grinding, in particular, place constant pressure on the joint. When stress and anxiety are added to the equation, the jaw muscles tense up even more, forcing the joint to work far beyond its normal limits.
Problems with bite alignment, missing teeth, or ill-fitting dentures can also disrupt jaw balance. Trauma to the jaw caused by accidents, impacts, or falls may damage the joint structure as well. Everyday habits that seem harmless such as chewing gum, biting pens, or chewing on only one side can gradually overwork the joint and pave the way for problems. In short, TMJ disorder often develops as a result of small factors that are overlooked for a long time.
How Is Temporomandibular Joint Disorder Diagnosed?
Temporomandibular joint disorder is usually not difficult to diagnose, and in most cases, a thorough examination is sufficient. The clinician carefully evaluates how the jaw opens and closes, whether any sounds occur during movement, and if there is tenderness in the jaw muscles. The patient’s symptoms how long they have been present and in which situations they worsen are also extremely valuable for making an accurate diagnosis.
In some cases, a closer look at the joint may be necessary. Imaging methods such as X-rays, MRI, or CT scans can be used when needed. However, advanced imaging is not required for every TMJ case. Often, a detailed examination combined with the right questions is enough to identify the source of the problem.
Treatment of Temporomandibular Joint Disorder
Treatment for temporomandibular joint disorder does not rely on a single approach applied to everyone. A personalized plan is created based on the cause of the problem, its severity, and how much it affects daily life. The good news is that the majority of people with TMJ disorder find relief through non-surgical methods.
The first step in treatment usually involves conservative and gentle approaches. Night guards, especially for individuals who clench or grind their teeth, help rest the jaw joint and allow the muscles to relax. Physical therapy and simple jaw exercises can gradually improve mobility and reduce pain. Managing stress is also a crucial part of treatment. Breathing exercises, relaxation techniques, and becoming aware of unconscious jaw clenching during the day can make a significant difference. Temporarily switching to softer foods can further reduce strain on the joint and support healing.
Comments are closed